NEWBORN FEEDING PREPARATION
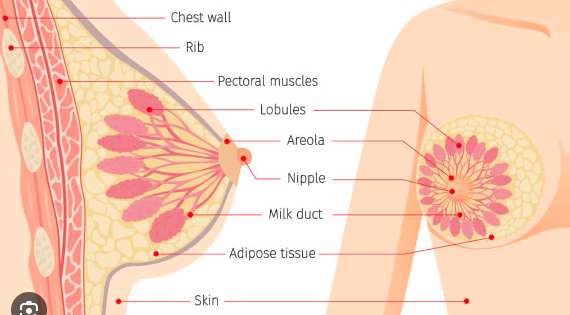
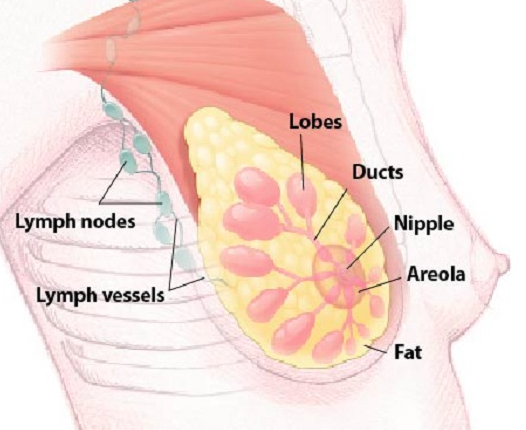
BREASTFEEDING ANATOMY & THE HORMONES OF BREASTFEEDING
See Video: Medical Animation: Breastfeeding
Prolactin + Oxytocin
HUMAN MILK
Colostrum– This is the early milk you will have immediately after birth (and sometimes in late pregnancy) that we call “liquid gold.” It is a yellowish or syrupy clear fluid, high in protein, lower in fat than mature milk and has a srong laxative effective to help remove meconium. It is rich in antibodies to protect baby from infections. The amount of colostrum your baby needs in the first few days is very small. At brith your baby’s stomach is very small (some say the size of a cherry, marble… small) and they only need about an ounce of colostrum per day, or about a teaspoon at each feeding. The most important thing to do to make sure your baby is getting what is needed, from day 1 through the first couple weeks, is to count pees and poops.
Milk starts to transition usually around day 3-4, but in some cases can take longer. Milk transitions slowly like a faucet from going from cold to warm. Transitional milk has a yellowish tint, is thinner and high in fat and calories, but lower in protein.
Mature milk is bluish white, more like skim milk and contains more calories and protein. Milk is primarily water and fat, with some protein (whey), carbohydrates (lactose), vitamin d, minerals, vitamins and antibodies. Babies needs fat for the brain and nervous system.
Normal Newborn Expectations
10-12 feedings per 24 hour time period
Every 1-3 hours.
PEES & POOPS
Counting and observing pees and poops is the only way to know in the early days (aside from weight checks) if you baby is getting what they need.
Some charts I like:
From Quebec Best Start ~ colorful pee and poop counting chart for the first weeks
Sleep Cycles:
Deep Sleep- Worst time to feed a baby, you can make lots of noise and they will not rouse. If baby is due for a feeding, take baby to mother skin-to-skin and often in about 20 minutes they will move to REM sleep
Light Sleep: REM, one of the best times to bring baby to the breast
Quiet Alert: fixed focused eyes, still body, also a great time for feeding
Active Alert: baby is growing restless, or active hands are coming to the mouth, open eyes with rooting. Still a good time to feed, but it’s time to move quickly.
Crying: Late stage hunger cue, tongue is lifted which is not an ideal place for latch
Skin to Skin (or Kangaroo Care)
From UNICEF’s Baby Friendly Initiative
There is a growing body of evidence that skin-to-skin contact after the birth helps babies and their mothers. The practice:
calms and relaxes both mother and baby
regulates the baby’s heart rate and breathing, helping them to better adapt to life outside the womb
stimulates digestion and an interest in feeding
regulates temperature
enables colonisation of the baby’s skin with the mother’s friendly bacteria, thus providing protection against infection
stimulates the release of hormones to support breastfeeding and mothering.
Skin-to-skin contact also provides benefits for babies in the neonatal unit, in that it:
improves oxygen saturation
reduces cortisol (stress) levels, particularly following painful procedures
encourages pre-feeding behaviour
assists with growth
may reduce hospital stay
improves milk volume if the mother expresses following a period of skin-to-skin contact, with the expressed milk containing the most up-to-date antibodies.
Breast/Chestfeeding Positioning & Latch Checklist
For latching:
baby’s head is tipped back
Baby’s hands are free and on either side of breast, free (if possible)
Bring baby close to breast
Wait (as much as is possible) for baby to open mouth wide
Then bring baby in strongly (smushed in, so nose is touching breast)
Baby’s position while feeding:
Baby’s belly to you belly, face to breast
Nose smushed in (touching the breast, in most cases)
A lot of the areola is symmetrically in the mouth
Head is still tipped back so jaw can move freely (pull baby in closer by pressing on baby’s shoulder blades with the back of your hand)
Hold baby securely
Look for:
Fish lips (Lips turn up, especially the bottom lip)
Rocking movements in the jaw, pulsing movement in temples
Wide obtuse angle at the side of the mouth
Watch for sucks and swallows
You can coax and help baby throughout the feed by massaging breast, gently touching to the face, talking or singing to baby, or gentling blowing on the face
Ending the feed:
Let baby finish the feed (whenever possible)
Look at nipples immediately after baby releases to see nipple shape
Bring baby upright to help and attempt to burp
Let nipples air dry
Some mild pain and cracking in the beginning is common, ongoing pain and deep cracking with blood may require antibacterial treatment. Pain n the first 30 seconds to 1 minute of feed is often due to cracked nipples (bear with this) and keep going. Pain throughout the feed may have to do with latch, try re-latching.
See Videos GOOD FEEDING VS. “NIBBLING” from the International Breastfeeding Center
MORE TO DISCUSS:
Sitting Positions
BREASTFEEDING IS A FULL BODY ACTIVITY FOR MOTHER AND BABY!!!!
Things I do like about the drawings below, the images do not show
the mothers feet or legs
the furniture the mother is sitting
the use props and pillows
Upright: Cross cradle, cradle, footbal
Laid Back
Side Lying
Photos and more descriptions:
Also see: Ina May’s Guide to Breastfeeding (book) or The Womanly Art of Breastfeeding (book from LLL)
Nursing pillows: My Breast Friend
Hand-expression + alternative feeding methods for the first week (syringe, spoon, cup)
See Video on Hand Expression (Keep in mind, these women are expressing mature milk and not colostrum. A teaspoon is a great amount of colostrum.)
Workshop on hand expression: Learn to Go Milk Yourself with Francie Webb
Engorgement
See hand expression video for a visual of an engorged breast
use warm compresses, hand expression
washed, dried and organic cabbage leaves can be nice for pain relief
Pumping
Some basics:
Great explaination on pump settings
For determining flange size: Nipple queen ruler or Silicone Measuring Tool
Storing Breast Milk Resources
Kelly Mom Printable Storage Instruction Sheet
Local IBCLC referrals will be provided if needed
BENEFITS OF BREASTFEEDING + HUMAN MILK
FROM THE CDC:
Breastfeeding can help protect babies against some short- and long-term illnesses and diseases.
Breastfed babies have a lower risk of asthma, obesity, type 1 diabetes, and sudden infant death syndrome (SIDS). Breastfed babies are also less likely to have ear infections and stomach bugs.Breast milk shares antibodies from the mother with her baby.
These antibodies help babies develop a strong immune system and protect them from illnesses.Mothers can breastfeed anytime and anywhere.
Breastfeeding can reduce the mother’s risk of breast and ovarian cancer, type 2 diabetes, and high blood pressure.
Other sources note:
Benefits to baby’s cognitive development and brain.
Benefits to baby’s GI system
Benefits to mother’s recovery by release of oxytocin, by promoting uterine contraction, bonding and relaxation
Decreased risk of diarrheal infections, allergies
NUTRITION & BREASTFEEDING
From Lily Nichols
First and foremorst
ALL BREAST MILK IS A PERFECT FOOD. THOSE WHO BREASTFEED SHOULD NOT EVER CHOOSE NOT TO BREASTFEED BECAUSE OF CONCERNS WITH THEIR DIET. Those who are unable to eat a nutritional dense diet still make the best food for their baby. According to Lily Nichols, “It’s all a superfood rich in immune boosting antibodies and easy to digest proteins, fats, and carbohydrates.” No one needs to eat a “perfect” diet during postpartum, as that can put alot of pressure on people during an already highly demanding time period. Additionally, as per Nichols “The whole process of breastfeeding is nothing short of a miracle, designed to help babies survive even if a mother is facing dire nutritional circumstances….Calories, protein, folate and most trace minerals are sufficient even in breast milk of undernourished women.”
That said, breastfeeding is nutritionally demanding, can lead to depletion of nutritions in those who nurse and more recent research does show that the quality of the food you eat, does impact breast milk content.
Nichols hares, One researcher, who examined B-vitamin content of breastmilk (and found it lacking), sums it up well,
“The overal picture that emerges is consistent across nutrients and points to an urgent need to improve the information available on breast milk quality.” – Lindsay Allen
Nichols also notes:
Choosing real food fats in lieu of margarine will prevent the transfer of harmful trans fats into breastmilk (and instead ensure the transfer all sorts of good fat-soluble vitamins) (AJCN, 2014).
Choosing animal foods sourced from grass-fed and/or pasture-raised animals will provide more nutrients and fewer pesticide residues.
Making sure your vitamin D levels are optimal will increase the vitamin D transferred into your breastmilk. (J Hum Lact, 2013)



